- Overview
- Summary of Types of Bone Mineral Density Tests
- Patients Recommended for Bone Mineral Density Measurements
- Medicare Guidelines for Bone Densitometry
- Understanding the Results of Bone Mineral Density Tests: T-score and Z-score
Technologists often diagnose osteoporosis by measuring a patient's bone mineral density (BMD). Bone mineral density measures the amount of calcium in regions of the bones. Most methods for measuring BMD (also called bone densitometry) are fast, non-invasive, painless and available on an outpatient basis. Bone densitometry can also be used to estimate a patient's risk of fracture. BMD methods involve taking dual energy x-rays (DEXA) or CT scans (Osteo CT or QCT) of bones in the spinal column, wrist, arm or leg. These methods compare the numerical density of the bone (calculated from the image), with empirical (historical) data bases of bone density to determine whether a patient has osteoporosis, and often, to what degree.

A patient receives a DEXA bone densitometry exam (image courtesy of Hologic)
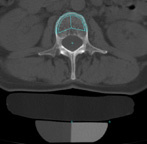
Cross-sectional image showing CT measurement of bone mineral density. A computer program compares the density of the patient's spinal vertebrae (outlined in turquoise) with a special reference device placed under the patient during the exam.
DEXA (Dual Energy X-ray Absorptiometry) is the most widely available method of bone densitometry, and most insurance plans will cover the cost for the test, given that certain medical indicators are present. Bone mineral density measurement with DEXA is painless, and requires no injections, invasive procedures, sedation, special diet or any other advance preparation. During a DEXA exam, the patient lies fully clothed on a padded table while the system scans one or more areas of bone (usually the lower spine or hip). The entire exam typically takes just a few minutes to complete. While DEXA uses x-rays, the radiation dose is less than during a chest x-ray. Each patient's bone density is plotted against the "normal" for a healthy young adult or against age matched control data. A radiologist or other physician then interprets the data and creates a concise report on the status of the patient's bone density.
Laboratory tests that measure the amount of collagen in urine samples can indicate bone loss. Lab tests may also be used in conjunction with DEXA or other methods of bone densitometry to diagnose osteoporosis.

A woman sits while receiving ultrasound bone densitometry by measurement of her heel.
New methods of measuring osteoporosis using ultrasound have also been developed. One such ultrasound system measures BMD at the patient's heel and takes about a minute. The ultrasound systems for testing osteoporosis are smaller and less expensive than traditional DEXA systems. These systems have recently received US Food and Drug Administration (FDA) clearance. The hope is that this more compact, lower cost system will allow this vital diagnostic test to become more widely available in the future. By primarily measuring peripheral sites such as the heel, ultrasound densitometry may not be as sensitive as techniques such as DEXA or QCT that measure the spine or hip since the heel may be normal in bone density even when central sites such as the hip or spine are already significantly abnormal.
Further, density changes in the heel occur much slower than in the hip or spine. Therefore ultrasound densitometry should not be used to monitor a patient's response to therapy. However, the new ultrasound densitometry systems will allow many more people access to bone densitometry and potentially diagnose osteoporosis before a traumatic fracture occurs.
- Ultrasound measures the heel
- DEXA (Dual Energy X-ray Absorptiometry) measures the spine, hip or total body
- SXA (single Energy X-ray Absorptiometry) measures the wrist or heel
- PDXA (Peripheral Dual Energy X-ray Absorptiometry) measures the wrist, heel or finger
- RA (Radiographic Absorptiometry) uses an X-ray of the hand and a small metal wedge to calculate bone density
- DPA (Dual Photon Absorptiometry) measures the spine, hip or total body
- SPA (Single Photon Absorptiometry) measures the wrist
- QCT (Quantitative Computed Tomography) measures spine or hip
The accuracy of bone mineral density test is high, ranging from 85% to 99%. DEXA is the most widely available BMD test and its accuracy, although QCT (and ultrasound) also show promise as effective tools in measuring BMD. However, QCT is not widely available and delivers more radiation to the patient than DEXA.
- Post-menopausal women with at least one additional risk factor (other than menopause).
- All women older than 65 regardless of risk factors.
- Post-menopausal women who present with fractures.
- Women considering therapy for osteoporosis, if bone mineral density (BMD) testing would affect the decision.
- Women who have been on hormone replacement therapy (HRT) for prolonged periods of time.
- Estrogen deficient women at clinical risk for osteoporosis.
- Individuals with vertebral abnormalities.
- Individuals receiving, or planning to receive, long-term glucocorticoids.
- Individuals with primary hyperparathyroidism.
- Individuals being monitored to assess the response of efficacy of an approved osteoporosis drug therapy.
- Medicare will only reimburse when BMD tests are ordered by the treating health care provider.
- Frequency of BMD testing is once per two years.
- Benefit applies to all Medicare patients including managed care programs.
- Non-Medicare payers may have different guidelines.
Bone mineral density (BMD) tests are performed to determine whether a patient has osteoporosis or osteopenia, a low bone mass that puts her at risk for osteoporosis. To make this determination, the technologist will calculate the patient's T-score. The World Health Organization (WHO) established the criteria for determining the T-score.
To calculate a patient's T-score, physicians subtract the patient's measured BMD from a BMD reference range of women in their thirties (YN = young normal). Around age 35, bone mass is usually at its peak and fracture risk is at its lowest. This figure is then divided by the standard deviation (SD).
T Score = (BMD - YN) / SD
By determining a patient's T-score, the physician will see whether a woman has or is at risk for osteoporosis:
| T-Score: WHO Criteria for Osteoporosis in Women | |
| Normal | BMD > -1.0 below the young adult reference range |
| Low Bone Mass (Osteopenia) | BMD is -1.0 to -2.5 SD below the young adult reference range |
| Osteoporosis | BMD < -2.5 SD below the young adult reference range |
| Severe Osteoporosis | BMD < -2.5 SD below the young adult reference range and the patient has one or more fractures |
As a rule, a patient's fracture risk doubles for every SD (standard deviation) below the young adult reference range. For example, if a patients' T-score is -2 SD, she is at four times greater risk of a fracture than a young woman at peak bone density.
Physicians may also measure a patient's Z-score with a bone mineral density test. The Z-score compares the patient's measured BMD to the average BMD measurement for the patient's age and sex. The Z-score is not used to confirm a diagnosis of osteoporosis because a favorable BMD measurement (compared to the average BMD measurement for the patient's age group) does not mean the patient is not at risk for osteoporosis.
Bone mineral density increases until around age 35 and then levels off until menopause. During the first six to eight years of menopause, there is a sharp decline in bone mineral density. It is estimated that between 1% and 5% of bone density is lost at this time. The higher a woman's overall bone density, the less she will be affected when she loses bone density at menopause.



